Providers
In this issue
- Top News
- Hot Topics
- Clinic Spotlight
- Sophia Meyer Family Medicine
- Save the Date!
- Second Quarter PCF Webinar May 15th and 16th
- Personal Touch
Top News
2024 Primary Care First Enrollment
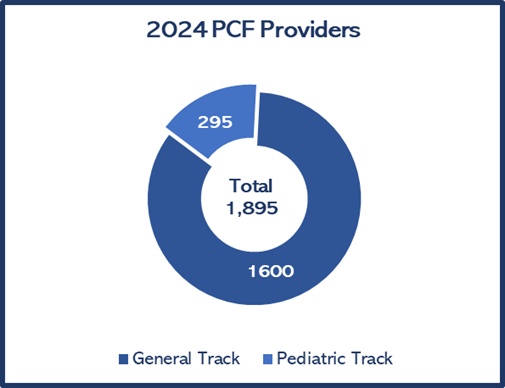
We are excited to announce that there are more providers participating in PCF than we had in PCF and PCMH combined in 2023! We appreciate the commitment of these providers to provide high quality care to their patients.
n 2024 there are 295 providers in the Pediatric Track and 1,600 providers in the General Track.
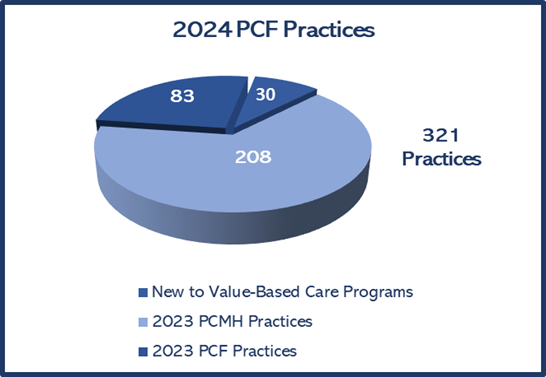
There are a total of 321 practices participating in PCF in 2024. That total includes 83 returning PCF practices, 208 former PCMH practices, and 30 practices new to value-based care programs. We applaud these providers and practices for their involvement in value-based care
Care Delivery Assessment
The Arkansas Blue Cross and Blue Shield Care Delivery Assessment is a tool used by the Primary Care Representatives to understand the practice patterns of the clinics participating in the Primary Care Value Based program. Prior to the 2024 program year, all clinics were required to complete the survey. For 2024, we only required the clinics that were new to the program to complete the assessment.
The questions are designed to assess each clinic’s care delivery model to form a baseline. Information from the CDA will help influence training and identify coaching opportunity.
Primary Care First clinics have implemented several of the comprehensive functions of an advanced care delivery model. Some notable results are listed below.
Access is so important for patients because being able to address a problem and give advice in a timely manner helps to improve patient outcomes and reduce ED visits for non-urgent needs, thus helping to lower utilization of higher cost settings. The results of the survey showed that 95% of our practices offer 24-hour real-time support from a member of their care team and 76% always offer same or next day appointments.
A Social Determinants of Health (SDoH) screening tool is a questionnaire that gathers information from patients about their general social needs in addition to their immediate health needs. When patients are screened for social needs at their medical appointments, healthcare providers can identify ways to address those needs and their root causes. The reason a clinic should screen for SDoH is simple: If you don’t ask, you won’t know. And if you do not know about a patient's social needs, you cannot address them. 92% of our clinics screen for social needs. Along with the social needs that are normally screened for such as: food insecurity, housing instability, utility needs, and transportation, we also found it very interesting that several of our clinics screened for: dental, vision, hearing, mental health, substance abuse, grief counseling, prescription assistance, home care and therapy services needs of their patients.
Transitions of care is important for helping to reduce unnecessary ED and Inpatient readmissions. We found that only 1 practice is not following up with patients discharged from the hospital. We had 62% of clinics report that they follow up with patients within 24-48 hours of discharge. We are very pleased that so many clinics across the state follow up with patients in a timely manner to address any needs or questions the patient may have from their hospital visit. The majority of our practices complete a medication reconciliation during their follow up. Reconciling medications during a transitions of care follow up call is very helpful to address problems quickly and improve patient outcomes.
An action plan outlines one or more easy steps a patient can take to attain a health goal, such as improving self-management of a chronic condition. 81% of practices have action plans for their patients’ chronic conditions. Some of the actions plans that clinics have implemented outside of the common chronic conditions are ADHD, Chronic UTI, and seizures. We have 65% of practices that have a process in place to monitor and follow-up on action plans. We want to encourage you to develop a workflow to monitor and follow-up if you do not have one in place.
In 2024, we developed a new measure around screening for behavioral health needs. 94% of practices reported screening for behavioral health needs. There are several models for integrating behavioral health services into your practice. The Collaborative Care Model is a model in which primary care providers, care managers, and psychiatric consultants collaborate to provide care and monitor patient’s progress. The majority of practices reported that this is the model they have integrated.
87% of our practices have a quality improvement team that receives and reviews clinical quality gaps, health care utilization, total cost of care, and other outcome data for patients. We had 30% of practices report that their provider and care team members, and/or their quality improvement team review the data daily, 39% review the data monthly, and 13% review quarterly. The APP Care Management portal updates monthly for you to be able to view your quality and utilization data. We want to encourage you to log in to the portal and review and work your data at least monthly.
Using these care delivery components, Primary Care First practices provide comprehensive and continuous care, reducing patients’ complications and overutilization of higher cost settings, leading to higher quality of care and reduced spending.
If you have any questions about any of the components of the care delivery model please refer to our program manual, review the slides that were shared at the value-based training in February, or reach out to your coach.
Hot Topics
Community Health
A Community Health Worker (CHW) is a frontline public health worker who is a trusted member of and/or has a strong understanding of the community served. This trusting relationship helps the CHW to act as a connector between health and social services and the community. A CHW helps to increase access to care and to improve the quality of medical and social services and cultural competence (i.e., understanding the cultural differences, values, and beliefs of people in need) during service delivery.
Community Health Worker is an umbrella term and a CHW can go by many different names including peer educator, patient navigator, community outreach specialist, health advocate, health promoter, etc.
A CHW helps to build individual and community capacity to empower people and communities to solve shared problems to improve individual lives and the community overall.
Several clinics across the state now have Community Health Workers to help their patient population with needs that may have been going unmet. They have seen the value in investing in CHWs and how they have had such a positive impact on the lives and wellbeing of their patients. One such clinic is Mainline Health Systems.
Mainline Health Systems has been in operation since 1978 and has grown over the years to provide comprehensive health and dental care to meet the needs of the communities across South Arkansas. They now have over 30 locations throughout Ashley, Bradley, Chicot, Cleveland, Desha, Drew, Grant and Lincoln counites.
One service they began offering about two years ago is providing Community Health Workers to their patients. They began with three CHWs and now have a total of 10. The Community Health Workers are able to assess the needs of the patients to see how they can best serve them. Once they assess the needs, then they begin the process of finding the resources that will best fit the patient’s needs and they will stay in contact with them until their needs are met. Patients are able to reach back out to the CHW if anything changes or if they have additional needs. Some of the services that the patients receive include help with housing, food, utilities, clothing, medicine, setting appointments and transportation. Patient’s lives are directly impacted by their needs being met on a daily or monthly basis because of the help they are receiving from the Community Health Workers. The number of patients they serve varies from week to week and month to month just depending on the needs of their patient population.
Since Mainline started this program, their patients have grown in the knowledge of what & how the Community Health Workers can help them and they have even become more comfortable with them coming into their homes and their lives. They have become family.
According to Barbara Davidson, CHW Coordinator for Mainline, CHW's do online training and continue with online training throughout the year.
“I believe that if we have been able to make "a small" difference in the lives of our patients we have succeeded....we have been able to get food to those who needed it, we have been able to get electricity/water turned back on for patients who have been without for weeks/months, we have been able to get patients in for doctor visits that haven't been in for years & get them back on the right track making sure that they continue in the right direction by keeping follow up visits & future appts.
In the summer of 2023 when temps were 102'/104' we were able to get a patient a window unit & help him close off some of his rooms in his house so that he could have relief from the heat. We have been able to get a patient's front door fixed so that it would shut correctly so that she could lock it & feel safe again in her own home. We had one patient that her husband was trying to work (he was their sole income) and take care of his wife feeding, clothing, medicines etc. We were able to get him set up with in-house help, meals on wheels, making our patient's life better & his life better. He told us that "He was on his last straw & didn't know what the future held" he was so relieved & so very thankful for the help.
I hope this gives you a small glimpse of the privileges that we as CHW's get to have in the lives of our patients.

When we see those grins, get the heartfelt hugs, tears of happiness from the ones we get to help it will make your heart smile & there is no better feeling than that.
Being a CHW isn't a job it’s a calling....”
Mainline Community Health Worker Coordinator
Barbara Davidson
(870) 538-3355 Ext. 10015
Clinic Spotlight: Sophia Meyer Family Medicine

Sophia Meyer Family Medicine Clinic, located in Van Buren, has been a long-time member of the Arkansas Blue Cross Blue Shield Value-based programs. One of the ways they expand their primary care functions is using social media to share and communicate with their followers, their patients, and families.
They use their Facebook page for patient education and make a point to post about which awareness month it is, such as Colon Cancer Awareness month in March, Mental Health Awareness month in May, and Breast Cancer Awareness month in October. During these months, they post about prevention and the importance of testing, along with statistics and offers to schedule needed testing for their patients. During COVID and Flu and RSV seasons, they share local statistics and recommendations on their Facebook page to keep the community up to date.
The clinic uses Facebook to update on things happening in the clinic such as staff birthdays with pictures of cakes, sharing clinic door decoration pictures during the holidays, posting notices when providers are out of the office, or inclement weather closings and community weather advisories, letting their patients know about patient appreciation activities, and even posting job openings and opportunities in the clinic.

Sophia Meyer Family Medicine Clinic, located in Van Buren, has been a long-time member of the Arkansas Blue Cross Blue Shield Value-based programs. One of the ways they expand their primary care functions is using social media to share and communicate with their followers, their patients, and families.
They use their Facebook page for patient education and make a point to post about which awareness month it is, such as Colon Cancer Awareness month in March, Mental Health Awareness month in May, and Breast Cancer Awareness month in October. During these months, they post about prevention and the importance of testing, along with statistics and offers to schedule needed testing for their patients. During COVID and Flu and RSV seasons, they share local statistics and recommendations on their Facebook page to keep the community up to date.
The clinic uses Facebook to update on things happening in the clinic such as staff birthdays with pictures of cakes, sharing clinic door decoration pictures during the holidays, posting notices when providers are out of the office, or inclement weather closings and community weather advisories, letting their patients know about patient appreciation activities, and even posting job openings and opportunities in the clinic.
Save the Date
- PCF Second Quarter Webinar May 15th and 16th. Registration links will be sent via email.
Personal Touch: Sonya Martin

Sonya Martin is the Primary Care Senior Data Analyst. Sonya has been with Arkansas Blue Cross Blue Shield for a little over 6 years and has been in the Primary Care Department for over 5 years. Sonya started her career in IT working as a programmer/Analyst and has continued in that field for over 20 years.
Sonya lives in Little Rock and is the primary caretaker for her parents. She also has 2 dogs Bentley and Birdie.
When talking about her passion for IT, Sonya states, “I enjoy lifting the hood and looking at all the nuts and bolts that make a program like Primary Care First work. I enjoy the challenges from all the intricacies and process flows needed to make sure everything is setup correctly to finding the needle in the haystack when something doesn’t go as planned. Working in the Primary Care Department has shown me the importance of Value-Based Care. I want to see all of our members across the state benefit from keeping healthcare costs down, producing better healthcare outcomes, and improve overall health and well-being.”
Primary Care Team
- Missy Davis, Director
- Adam Whitlock, Manager
- Amanda Barber, Primary Care Representative
- Harry Bounds, Primary Care Representative
- Melissa El Houri, Primary Care Representative
- Leisa Hobson, Project Coordinator
- Dana King, Primary Care Representative
- Xinyu Li, Data Analyst
- Sonya Martin, Senior Data Analyst
- Tina Zimmerman, Primary Care Representative
