Providers

In this issue
- Top News
- Hot Topics
- Metric Spotlight
- Behavioral Health Screening
- Clinic Spotlight
- 1st Choice Healthcare
- Save the Date!
- Value-Based Program Training
- Care Delivery Assessment
- Personal Touch
Top News
A Slice of Value Conversations

A Slice of Value Conversations bring a local perspective to value-based primary care. Hosted by Adam Whitlock with Arkansas BlueCross BlueShield, you will hear real stories from primary care providers, population health team members, and others caring for patients on the front lines of healthcare in Arkansas. Through the conversations you will encounter patient experiences, discover the “why” behind each guest’s reason for providing high quality care, and feel inspired to implement best practices that can equip you and your organization to make the most of value-based primary care.
Episodes 1 and 2 are available now!
- Episode 1 features Dr. Jason Lofton from Lofton Family Practice.
- Episode 2 features Kenderia Perry from North Central Arkansas Medical Associates.
You can access A Slice of Value Conversations here
2024 Primary Care First

In 2024, Primary Care First will be the only Primary Care Value-Based Program offered by Arkansas BlueCross Blue Shield. Primary Care First (PCF) is a value-based program that utilizes a patient-centered medical home care delivery model and an advanced payment model.
The goal of Primary Care First is to reduce patients’ complications and overutilization of higher cost settings, leading to higher quality of care and reduced spending.
For 2024, there are 322 practices and 1,866 providers participating in PCF. Primary Care First fosters practitioner independence by increasing flexibility for primary care, providing participating practitioners with the freedom to innovate their care delivery approach based on their unique patient population and resources. Primary Care First rewards participants with additional revenue for taking on limited risk based on easily understood, actionable outcomes.
During 2023, we listened to participating practices and held several provider forums to gain input on Primary Care First. We made some changes to PCF based on feedback we received.
- Wellness codes: Providers and Arkansas Blue Cross agree that preventive visits are very important. For 2024, wellness codes will NOT be subject to the fee-for-service reduction and will be paid at the regular contracted rate. As a reminder, there is no cost-share to members for wellness visits. Wellness visits for children and adolescents are Quality metrics in the Pediatric track. It is a good practice to always check eligibility and benefits.
- Payment structure: The payment structure will be aligned for both General and Pediatric tracks with the removal of wellness codes.
- Utilization and Quality:
- Utilization Performance Adjustment: Practices meeting utilization targets will be rewarded with positive adjustments to care management fees. Practices who fail to meet at least one utilization metric will receive a negative adjustment to care management fees. Utilization performance is measured and adjusted on a quarterly basis.
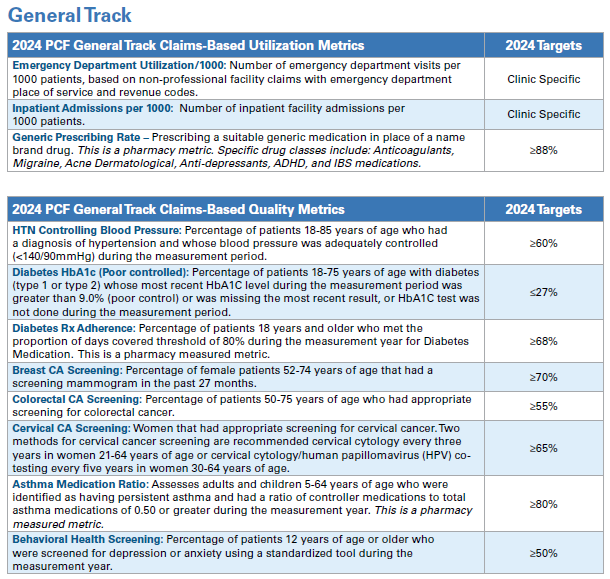
NEW for 2024:
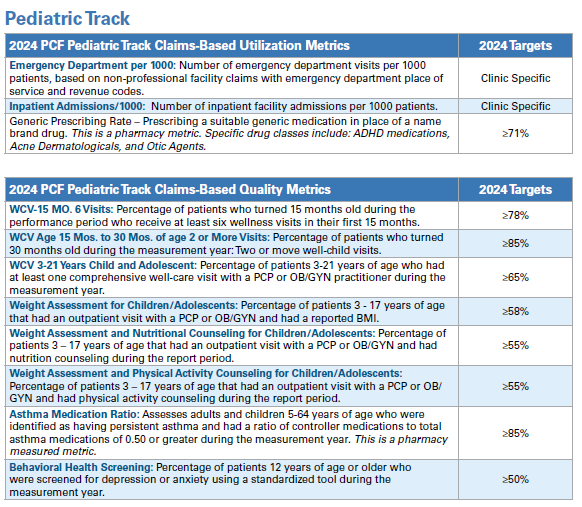
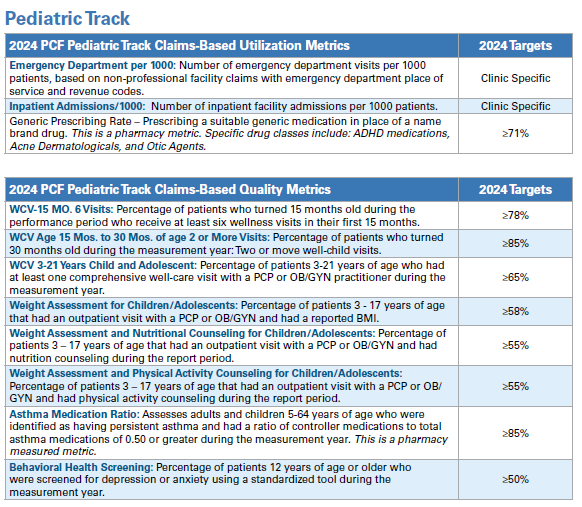
- General Track or Pediatric Track: In 2024, providers have the option to select the track that aligns with the majority of their patient population. Providers in the General track will be assessed on the Utilization and Quality metrics for the General Track, and providers in the Pediatric track will be assessed on the Utilization and Quality metrics for the Pediatric Track.
- Inpatient Admission targets have been adjusted to account for newborn admissions.
- New for 2024 is the addition of a Behavioral Health Screening metric. This metric will be in both the General track and the Pediatric track Quality Metrics.
- The Antidepressant Medication Management metric is removed for 2024.
- The Pediatric URI metric is also removed for 2024.
- Wellness visit codes are not subject to PCF FFS reductions.
Dates to remember:
- 2024 PCF Value-Based Training schedule:
- February 1, 2024, 9:00 - 11:00 at USAble Corporate Center, 320 West Capitol Ave., Little Rock, AR
- February 6, 2024, 9:00 - 11:00 virtual.
- Care Delivery Assessment will be sent out in February via Survey Monkey.
Hot Topics
January is Cervical Cancer Awareness Month!
January is Cervical Cancer Awareness Month and is a perfect opportunity to reach out to patients due for cervical cancer screenings. You can find a list of patients due for cervical cancer screening on the APP Care Management Portal or through your EHR. The goal of screening for cervical cancer is to find precancerous cervical cell changes early when treatment can prevent cervical cancer from developing. Cervical cancer found at an early stage is usually easier to treat. By the time symptoms appear, cervical cancer may have begun to spread, making treatment more difficult.
Cervical cancer screening is a quality metric for the General Track. The metric assesses the percentage of women 21-64 years of age who had appropriate screening for cervical cancer during the measurement period. This can be accomplished by cervical cytology services during the 36 months prior to the end of the reporting period OR had cervical cytology with an HPV test within 60 months prior to the end of the reporting period. You can run a list of your patients needing cervical cancer screening from the Care Management portal or through your EHR. If you find a patient on the care management portal that has had a hysterectomy with no residual cervix, you can have that patient excluded either by coding absence of cervix or by the attestation process on the Care Management Portal.
February is American Heart Month!

February is American Heart Month, a time to focus on cardiovascular health. CVD and CVD mortality are increasing in working-age adults, and black adults die from heart disease at a rate two times higher than white adults. This is a perfect time to follow up with patients that have hypertension. Schedule follow-up visits or wellness visits to help patients manage their blood pressure, cholesterol, eat healthier, reduce stress and quit smoking. Controlling high blood pressure is a quality metric for the General Track. To report blood pressure control, include CPT II codes for systolic and diastolic readings on your claims.
| CPT II Codes to be used on Claims | |
|---|---|
| 3074F | Systolic ‹ 130 mm Hg |
| 3075F | Systolic 130 – 139 mm Hg |
| 3077F | Systolic ≥140 mm Hg |
| 3078F | Diastolic ‹ 80 mm Hg |
| 3079F | Diastolic 80 – 89 mm Hg |
| 3080F | Diastolic ≥90 mm Hg |
March is Colorectal Cancer Awareness Month!

Raising awareness for colorectal cancer is critical to saving lives. Colorectal cancer is the third most common cancer type worldwide; in 2020, almost 2 million cases were diagnosed. It is the second most common cause of cancer death, leading to almost 1 million deaths per year. This is despite the fact that effective screening techniques exist that could reduce the number of deaths from this disease. Colorectal Cancer Awareness Month is observed in March to highlight the importance of screening for colorectal cancer as well as to promote healthy lifestyle habits that can decrease a person’s risk of developing colorectal cancer.
Colorectal cancer screening is a quality metric for the General Track. This metric assesses the percentage of adults 46-75 years of age who had colorectal cancer screening. This can be accomplished by an FOBT during the measurement year, FIT-DNA within 36 months of the end of the measurement year, flexible sigmoidoscopy or CT Colonography 5 years prior to the end of the measurement period OR a colonoscopy within 10 years of the end of the measurement period. You can see a list of your patients needing colorectal cancer screening on the Care Management Portal. Since the colorectal screening can go back as far as 10 years, there is a process in the Care Management Portal to attest that your patient had a colorectal cancer screening if you have the result in the medical record.
Metric Spotlight: Behavioral Health Screening
The only new Quality metric for 2024 will be the Behavioral Health Screening for both the General and Pediatric tracks. Behavioral and mental health affects 1 in 5 adults in the United States every year. Of those, more than 40% of people with mental disorders did not seek any treatment in the prior year.
Only 6% of people seek treatment from a mental health provider, but 80% of people go to primary care. With that in mind, you can see how the PCP reaches many more people. By integrating behavioral health screening in primary care, providers have the opportunity to identify patients with depression or anxiety. Many patients won’t come to the provider and just say, “I’m depressed.” They may present with fatigue or other symptoms. By screening all patients ages 12 and above, previously undiagnosed patients with depression or anxiety can be discovered, and the patients can receive the treatment they need to improve overall health.
Behavioral Health Screening: Percentage of patients 12 years of age or older who were screened for depression or anxiety using a standardized tool during the measurement year.
Metric specifications: Patients ages 12 or older screened for depression or anxiety during the 12-month reporting period, using a standardized screening tool.
Codes to be used on claims:
ICD-10 Codes
- Z13.31
- Z13.32
- Z13.39
Exclusions:
- Patent is in hospice care or
- Patient has a history of bipolar disorder or
- Patient has a diagnosis of depression or anxiety that began during the year prior to the measurement period.
Examples of standardized screening tools include PHQ2, PHQ9, GAD-7, EHR-based screener, or other standardized screening tool.
Screening for behavioral health should be considered mental health vital signs. Practices can include screening as part of the usual patient intake, just like blood pressure, height, weight, etc. Not only does this allow the provider to identify mental health needs, but it also decreases the stigma of mental health.
Screening results should be entered into the EHR for the provider to review. Providers will review the screening results and treat or refer the patient as appropriate. If a patient is referred to a mental health provider, implement a process to track those referrals to make sure the patient has received the treatment they need.
Clinic Spotlight: 1st Choice Healthcare

1st Choice Healthcare is a Federally Qualified Health Center (FQHC) serving six counties in northeast Arkansas, with 32 medical providers and 4 licensed clinical social workers. They currently have six clinics located in Clay, Greene, Randolph, Lawrence, Sharp and Fulton Counties, as well as a mobile unit. 1st Choice Healthcare is recognized as a Patient Centered Medical Home through the National Committee for Quality Assurance (NCQA) and holds ambulatory and laboratory accreditation from Joint Commission.
1st Choice Healthcare has integrated behavioral health. Since behavioral health screening is a new metric for PCF in 2024, read about some of their processes below:
Behavioral Health Screening – 1st Choice is actively working through collaborative projects to improve the number of patients 12 and older who are screened on an annual basis for depression at their medical visits. The PHQ-2 is used for the initial screening and, if positive, individuals 12 – 17 receive a PHQ-A and those 18 and above receive a PHQ-9. In addition, 1st Choice also uses other screening instruments, such as the GAD-7 for anxiety screening. Using the Audit-C and Drug Questionnaire, medical personnel also conduct alcohol and drug screenings. 1st Choice behavioral staff also utilize the PCL-5 for PTSD (posttraumatic stress disorder) and the MDQ for mood disorders as additional screening tools. They have 4 LCSWs and 1 RN on their behavioral health team. They screen for depression, anxiety, and social determinants of health at every initial appointment. Since starting integrated behavioral health care, they have provided access to behavioral health care for more than 1200 new patients.
- If you have a positive screen, what do you do? The primary care provider may initiate medications, if appropriate, and/ or provide education regarding management of a newly diagnosed behavioral health issue. Additionally, the primary care provider may initiate an internal or external referral for behavioral health services if the depression screening results are positive. If necessary, same-day care can be given by the behavioral health provider in the form of a warm handoff, a new patient appointment, or a crisis screening in emergent situations. Behavioral health providers are always available to facilitate warm hand-offs from our medical staff. Behavioral health providers are co-located in the clinic for real-time consulting. When a warm handoff happens, the behavioral health provider briefly interacts with the patient to develop rapport, and same-day services may be provided if warranted. Telehealth from another clinic can be used if a behavioral health provider is not in that clinic.
- What processes or workflows did you implement or change? Primary care and behavioral health have been included in workflow modifications at 1st Choice Healthcare. In four of our six clinics, there is an embedded behavioral health provider, and we intend to grow the workforce. As a member of the care team, the behavioral health provider works closely with primary care providers. Real-time assistance is offered for any behavioral health issue that may arise in the clinic. Medical and behavioral health both share the same EMR, with additions added for behavioral health to include software to complete treatment plans and track patients. In addition, we added a security setting to make all behavioral health notes confidential.
- Behavioral Health Screening will be a new quality metric in 2024. What advice would you give to other clinics as they prepare to start screening? Inform your clinic first about the significance of behavioral health screening for primary care patients. Positive outcomes for depression are promoted by early identification and intervention, according to data. It is crucial to have a systematic process for patients who screen positive, which includes evidence-based methods and support systems. It is also important to provide personnel with proper training on how to administer behavioral health screenings.
- What are some initial struggles that you encountered and how have you overcome them? Finding behavioral health providers for every clinic location was challenging at first and is still challenging now. In clinics without behavioral health providers, we offer telehealth. Our second issue was creating and integrating a behavioral health documentation platform within an electronic medical record. Behavioral health care management software and behavioral health templates have been used to solve this. The final obstacle was shifting the clinic's philosophy from medical only care to integrated behavioral health. To overcome this barrier, behavioral health providers actively collaborate with medical staff to show value in integrated care.
1st Choice Healthcare has referral coordinators in all clinic locations. Coordinators track referrals and medical records, ensuring continuity of care from the start to the finish.
A new clinic in Pocahontas opened in December 2023, and another clinic will be added in Highland. While not every clinic has LCSWs, they utilize telehealth to fill the gap to provide behavioral health services.
If you have any questions for 1st Choice Healthcare, contact Lyle Kennedy, RN at 1st Choice Healthcare, Inc., 1001 N. Missouri Ave. Corning, AR 72422, phone 870-857-3334.
Save the Date
- 2024 Value-Based Program Training February 1 (Little Rock) and February 6 (virtual)
- Care Delivery Assessments in February
Personal Touch: Tina Zimmerman

Tina M. Zimmerman, LPN, MHP is the Primary Care Representative for Northwest and North Central Arkansas. Tina has been with Arkansas Blue Cross Blue Shield for almost 10 years and been in the Primary Care Department for almost six years. Tina started her career in nursing working inpatient ortho/med surg then expanded her career to include, long term care, clinic nursing for both independent and system clinics, urgent care, teaching, and was in nurse management for 2 years prior to coming to Arkansas Blue Cross Blue Shield.
Tina lives in Conway and has two sons and one daughter and a granddaughter and a grandson. She is a true die-hard Arkansas Razorbacks fan and loves to spend time with her family.
When talking about her passion for nursing and healthcare, Tina states, “My father passed away at the very young age of 52 of colon cancer, and my mom and my sister both have battled diabetes for years. I have seen firsthand how preventative screenings, chronic disease management, medication adherence, and patient accountability are so important, and how they can mean the difference between just living a life and living a good and happy life. I am a firm believer in closing gaps, transitions of care, and open communication between patients and healthcare providers. My hope is that I can help my clinics and all Arkansans to not only prevent and find issues early but be able to take control of their disease instead of it controlling them.”
Primary Care Team
- Missy Davis, Director
- Adam Whitlock, Manager
- Amanda Barber, Primary Care Representative
- Harry Bounds, Primary Care Representative
- Melissa El Houri, Primary Care Representative
- Leisa Hobson, Project Coordinator
- Dana King, Primary Care Representative
- Xinyu Li, Data Analyst
- Sonya Martin, Senior Data Analyst
- Tina Zimmerman, Primary Care Representative
About A slice of Value
Issue Archive
In this issue
- Top News
- Hot Topics
- Metric Spotlight
- Behavioral Health Screening
- Clinic Spotlight
- 1st Choice Healthcare
- Save the Date!
- Value-Based Program Training
- Care Delivery Assessment
- Personal Touch
Top News
A Slice of Value Conversations

A Slice of Value Conversations bring a local perspective to value-based primary care. Hosted by Adam Whitlock with Arkansas BlueCross BlueShield, you will hear real stories from primary care providers, population health team members, and others caring for patients on the front lines of healthcare in Arkansas. Through the conversations you will encounter patient experiences, discover the “why” behind each guest’s reason for providing high quality care, and feel inspired to implement best practices that can equip you and your organization to make the most of value-based primary care.
Episodes 1 and 2 are available now!
- Episode 1 features Dr. Jason Lofton from Lofton Family Practice.
- Episode 2 features Kenderia Perry from North Central Arkansas Medical Associates.
You can access A Slice of Value Conversations here
2024 Primary Care First

In 2024, Primary Care First will be the only Primary Care Value-Based Program offered by Arkansas BlueCross Blue Shield. Primary Care First (PCF) is a value-based program that utilizes a patient-centered medical home care delivery model and an advanced payment model.
The goal of Primary Care First is to reduce patients’ complications and overutilization of higher cost settings, leading to higher quality of care and reduced spending.
For 2024, there are 322 practices and 1,866 providers participating in PCF. Primary Care First fosters practitioner independence by increasing flexibility for primary care, providing participating practitioners with the freedom to innovate their care delivery approach based on their unique patient population and resources. Primary Care First rewards participants with additional revenue for taking on limited risk based on easily understood, actionable outcomes.
During 2023, we listened to participating practices and held several provider forums to gain input on Primary Care First. We made some changes to PCF based on feedback we received.
- Wellness codes: Providers and Arkansas Blue Cross agree that preventive visits are very important. For 2024, wellness codes will NOT be subject to the fee-for-service reduction and will be paid at the regular contracted rate. As a reminder, there is no cost-share to members for wellness visits. Wellness visits for children and adolescents are Quality metrics in the Pediatric track. It is a good practice to always check eligibility and benefits.
- Payment structure: The payment structure will be aligned for both General and Pediatric tracks with the removal of wellness codes.
- Utilization and Quality:
- Utilization Performance Adjustment: Practices meeting utilization targets will be rewarded with positive adjustments to care management fees. Practices who fail to meet at least one utilization metric will receive a negative adjustment to care management fees. Utilization performance is measured and adjusted on a quarterly basis.
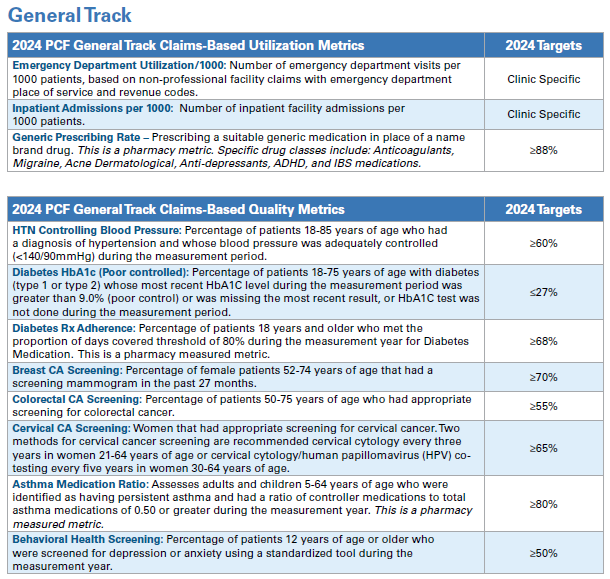
NEW for 2024:
- General Track or Pediatric Track: In 2024, providers have the option to select the track that aligns with the majority of their patient population. Providers in the General track will be assessed on the Utilization and Quality metrics for the General Track, and providers in the Pediatric track will be assessed on the Utilization and Quality metrics for the Pediatric Track.
- Inpatient Admission targets have been adjusted to account for newborn admissions.
- New for 2024 is the addition of a Behavioral Health Screening metric. This metric will be in both the General track and the Pediatric track Quality Metrics.
- The Antidepressant Medication Management metric is removed for 2024.
- The Pediatric URI metric is also removed for 2024.
- Wellness visit codes are not subject to PCF FFS reductions.
Dates to remember:
- 2024 PCF Value-Based Training schedule:
- February 1, 2024, 9:00 - 11:00 at USAble Corporate Center, 320 West Capitol Ave., Little Rock, AR
- February 6, 2024, 9:00 - 11:00 virtual.
- Care Delivery Assessment will be sent out in February via Survey Monkey.
Hot Topics
January is Cervical Cancer Awareness Month!
January is Cervical Cancer Awareness Month and is a perfect opportunity to reach out to patients due for cervical cancer screenings. You can find a list of patients due for cervical cancer screening on the APP Care Management Portal or through your EHR. The goal of screening for cervical cancer is to find precancerous cervical cell changes early when treatment can prevent cervical cancer from developing. Cervical cancer found at an early stage is usually easier to treat. By the time symptoms appear, cervical cancer may have begun to spread, making treatment more difficult.
Cervical cancer screening is a quality metric for the General Track. The metric assesses the percentage of women 21-64 years of age who had appropriate screening for cervical cancer during the measurement period. This can be accomplished by cervical cytology services during the 36 months prior to the end of the reporting period OR had cervical cytology with an HPV test within 60 months prior to the end of the reporting period. You can run a list of your patients needing cervical cancer screening from the Care Management portal or through your EHR. If you find a patient on the care management portal that has had a hysterectomy with no residual cervix, you can have that patient excluded either by coding absence of cervix or by the attestation process on the Care Management Portal.
February is American Heart Month!

February is American Heart Month, a time to focus on cardiovascular health. CVD and CVD mortality are increasing in working-age adults, and black adults die from heart disease at a rate two times higher than white adults. This is a perfect time to follow up with patients that have hypertension. Schedule follow-up visits or wellness visits to help patients manage their blood pressure, cholesterol, eat healthier, reduce stress and quit smoking. Controlling high blood pressure is a quality metric for the General Track. To report blood pressure control, include CPT II codes for systolic and diastolic readings on your claims.
| CPT II Codes to be used on Claims | |
|---|---|
| 3074F | Systolic ‹ 130 mm Hg |
| 3075F | Systolic 130 – 139 mm Hg |
| 3077F | Systolic ≥140 mm Hg |
| 3078F | Diastolic ‹ 80 mm Hg |
| 3079F | Diastolic 80 – 89 mm Hg |
| 3080F | Diastolic ≥90 mm Hg |
March is Colorectal Cancer Awareness Month!

Raising awareness for colorectal cancer is critical to saving lives. Colorectal cancer is the third most common cancer type worldwide; in 2020, almost 2 million cases were diagnosed. It is the second most common cause of cancer death, leading to almost 1 million deaths per year. This is despite the fact that effective screening techniques exist that could reduce the number of deaths from this disease. Colorectal Cancer Awareness Month is observed in March to highlight the importance of screening for colorectal cancer as well as to promote healthy lifestyle habits that can decrease a person’s risk of developing colorectal cancer.
Colorectal cancer screening is a quality metric for the General Track. This metric assesses the percentage of adults 46-75 years of age who had colorectal cancer screening. This can be accomplished by an FOBT during the measurement year, FIT-DNA within 36 months of the end of the measurement year, flexible sigmoidoscopy or CT Colonography 5 years prior to the end of the measurement period OR a colonoscopy within 10 years of the end of the measurement period. You can see a list of your patients needing colorectal cancer screening on the Care Management Portal. Since the colorectal screening can go back as far as 10 years, there is a process in the Care Management Portal to attest that your patient had a colorectal cancer screening if you have the result in the medical record.
Metric Spotlight: Behavioral Health Screening
The only new Quality metric for 2024 will be the Behavioral Health Screening for both the General and Pediatric tracks. Behavioral and mental health affects 1 in 5 adults in the United States every year. Of those, more than 40% of people with mental disorders did not seek any treatment in the prior year.
Only 6% of people seek treatment from a mental health provider, but 80% of people go to primary care. With that in mind, you can see how the PCP reaches many more people. By integrating behavioral health screening in primary care, providers have the opportunity to identify patients with depression or anxiety. Many patients won’t come to the provider and just say, “I’m depressed.” They may present with fatigue or other symptoms. By screening all patients ages 12 and above, previously undiagnosed patients with depression or anxiety can be discovered, and the patients can receive the treatment they need to improve overall health.
Behavioral Health Screening: Percentage of patients 12 years of age or older who were screened for depression or anxiety using a standardized tool during the measurement year.
Metric specifications: Patients ages 12 or older screened for depression or anxiety during the 12-month reporting period, using a standardized screening tool.
Codes to be used on claims:
ICD-10 Codes
- Z13.31
- Z13.32
- Z13.39
Exclusions:
- Patent is in hospice care or
- Patient has a history of bipolar disorder or
- Patient has a diagnosis of depression or anxiety that began during the year prior to the measurement period.
Examples of standardized screening tools include PHQ2, PHQ9, GAD-7, EHR-based screener, or other standardized screening tool.
Screening for behavioral health should be considered mental health vital signs. Practices can include screening as part of the usual patient intake, just like blood pressure, height, weight, etc. Not only does this allow the provider to identify mental health needs, but it also decreases the stigma of mental health.
Screening results should be entered into the EHR for the provider to review. Providers will review the screening results and treat or refer the patient as appropriate. If a patient is referred to a mental health provider, implement a process to track those referrals to make sure the patient has received the treatment they need.
Clinic Spotlight: 1st Choice Healthcare

1st Choice Healthcare is a Federally Qualified Health Center (FQHC) serving six counties in northeast Arkansas, with 32 medical providers and 4 licensed clinical social workers. They currently have six clinics located in Clay, Greene, Randolph, Lawrence, Sharp and Fulton Counties, as well as a mobile unit. 1st Choice Healthcare is recognized as a Patient Centered Medical Home through the National Committee for Quality Assurance (NCQA) and holds ambulatory and laboratory accreditation from Joint Commission.
1st Choice Healthcare has integrated behavioral health. Since behavioral health screening is a new metric for PCF in 2024, read about some of their processes below:
Behavioral Health Screening – 1st Choice is actively working through collaborative projects to improve the number of patients 12 and older who are screened on an annual basis for depression at their medical visits. The PHQ-2 is used for the initial screening and, if positive, individuals 12 – 17 receive a PHQ-A and those 18 and above receive a PHQ-9. In addition, 1st Choice also uses other screening instruments, such as the GAD-7 for anxiety screening. Using the Audit-C and Drug Questionnaire, medical personnel also conduct alcohol and drug screenings. 1st Choice behavioral staff also utilize the PCL-5 for PTSD (posttraumatic stress disorder) and the MDQ for mood disorders as additional screening tools. They have 4 LCSWs and 1 RN on their behavioral health team. They screen for depression, anxiety, and social determinants of health at every initial appointment. Since starting integrated behavioral health care, they have provided access to behavioral health care for more than 1200 new patients.
- If you have a positive screen, what do you do? The primary care provider may initiate medications, if appropriate, and/ or provide education regarding management of a newly diagnosed behavioral health issue. Additionally, the primary care provider may initiate an internal or external referral for behavioral health services if the depression screening results are positive. If necessary, same-day care can be given by the behavioral health provider in the form of a warm handoff, a new patient appointment, or a crisis screening in emergent situations. Behavioral health providers are always available to facilitate warm hand-offs from our medical staff. Behavioral health providers are co-located in the clinic for real-time consulting. When a warm handoff happens, the behavioral health provider briefly interacts with the patient to develop rapport, and same-day services may be provided if warranted. Telehealth from another clinic can be used if a behavioral health provider is not in that clinic.
- What processes or workflows did you implement or change? Primary care and behavioral health have been included in workflow modifications at 1st Choice Healthcare. In four of our six clinics, there is an embedded behavioral health provider, and we intend to grow the workforce. As a member of the care team, the behavioral health provider works closely with primary care providers. Real-time assistance is offered for any behavioral health issue that may arise in the clinic. Medical and behavioral health both share the same EMR, with additions added for behavioral health to include software to complete treatment plans and track patients. In addition, we added a security setting to make all behavioral health notes confidential.
- Behavioral Health Screening will be a new quality metric in 2024. What advice would you give to other clinics as they prepare to start screening? Inform your clinic first about the significance of behavioral health screening for primary care patients. Positive outcomes for depression are promoted by early identification and intervention, according to data. It is crucial to have a systematic process for patients who screen positive, which includes evidence-based methods and support systems. It is also important to provide personnel with proper training on how to administer behavioral health screenings.
- What are some initial struggles that you encountered and how have you overcome them? Finding behavioral health providers for every clinic location was challenging at first and is still challenging now. In clinics without behavioral health providers, we offer telehealth. Our second issue was creating and integrating a behavioral health documentation platform within an electronic medical record. Behavioral health care management software and behavioral health templates have been used to solve this. The final obstacle was shifting the clinic's philosophy from medical only care to integrated behavioral health. To overcome this barrier, behavioral health providers actively collaborate with medical staff to show value in integrated care.
1st Choice Healthcare has referral coordinators in all clinic locations. Coordinators track referrals and medical records, ensuring continuity of care from the start to the finish.
A new clinic in Pocahontas opened in December 2023, and another clinic will be added in Highland. While not every clinic has LCSWs, they utilize telehealth to fill the gap to provide behavioral health services.
If you have any questions for 1st Choice Healthcare, contact Lyle Kennedy, RN at 1st Choice Healthcare, Inc., 1001 N. Missouri Ave. Corning, AR 72422, phone 870-857-3334.
Save the Date
- 2024 Value-Based Program Training February 1 (Little Rock) and February 6 (virtual)
- Care Delivery Assessments in February
Personal Touch: Tina Zimmerman

Tina M. Zimmerman, LPN, MHP is the Primary Care Representative for Northwest and North Central Arkansas. Tina has been with Arkansas Blue Cross Blue Shield for almost 10 years and been in the Primary Care Department for almost six years. Tina started her career in nursing working inpatient ortho/med surg then expanded her career to include, long term care, clinic nursing for both independent and system clinics, urgent care, teaching, and was in nurse management for 2 years prior to coming to Arkansas Blue Cross Blue Shield.
Tina lives in Conway and has two sons and one daughter and a granddaughter and a grandson. She is a true die-hard Arkansas Razorbacks fan and loves to spend time with her family.
When talking about her passion for nursing and healthcare, Tina states, “My father passed away at the very young age of 52 of colon cancer, and my mom and my sister both have battled diabetes for years. I have seen firsthand how preventative screenings, chronic disease management, medication adherence, and patient accountability are so important, and how they can mean the difference between just living a life and living a good and happy life. I am a firm believer in closing gaps, transitions of care, and open communication between patients and healthcare providers. My hope is that I can help my clinics and all Arkansans to not only prevent and find issues early but be able to take control of their disease instead of it controlling them.”
Primary Care Team
- Missy Davis, Director
- Adam Whitlock, Manager
- Amanda Barber, Primary Care Representative
- Harry Bounds, Primary Care Representative
- Melissa El Houri, Primary Care Representative
- Leisa Hobson, Project Coordinator
- Dana King, Primary Care Representative
- Xinyu Li, Data Analyst
- Sonya Martin, Senior Data Analyst
- Tina Zimmerman, Primary Care Representative
